 Beginning Surgery ExperienceTwo weeks ago, Sam had hip replacement surgery at New England Baptist Hospital, a top nationally recognized orthopedic facility in Boston.
Beginning Surgery ExperienceTwo weeks ago, Sam had hip replacement surgery at New England Baptist Hospital, a top nationally recognized orthopedic facility in Boston.
My experience caring for Sam has given me a close-up view into how his needs (and mine as a caregiver) were met pre-, during and post- surgery. I saw firsthand how effectively his hospital collaborated with VNA Care for follow up in home nursing and PT.
As a consultant in the healthcare experience space, I’ve gathered insights from patients and caregivers about their healthcare journey. Through this caregiver experience, I’ve learned the nuances of the hip replacement processes, evaluated communications, information and tools to engage Sam and his caregiver, and envisioned opportunities to enhance his preparation and recovery.
In this post, I share some key insights with many “Gold Stars” for experiences that met/exceeded our expectations and a few “Magic Wand Wishes” for ways the provider could have executed a better patient and caregiver experience. Since hip replacement is an increasingly common and costly procedure, it is in the health system's best interest to optimize the experience.
With New England Baptist’s reputation as a top orthopedic facility, it is easy to see how they have earned high patient experience ratings. Their care team delivered a highly orchestrated process which anticipated Sam’s needs and made him feel comfortable and well-informed. There were however, opportunities for New England Baptist and partner VNA Care to improve the patient post-surgery experience, and the entire caregiver experience. Keep in mind that it is the caregiver on the front line supporting the patient following discharge, which in our situation was the same day as the surgery.
Pre-Surgery
A few weeks prior to surgery, Sam attended a 3-hour preadmission screening appointment where he reviewed surgery details with different care team members and had x-rays taken. Sam was given a New England Baptist branded cinch sack with a checklist about what to pack for the hospital. According to Sam, this appointment was a thorough and efficient process.
Closer to surgery, Sam received an email invite to attend a virtual “Hip Replacement Pre-Operative Class". Since Sam encouraged me as the caregiver to join him, I attended this 90-minute session and Q&A with about a dozen others (Note: Not sure why the other patient’s names were displayed in the Zoom meeting given HIPAA). Sam also received a series of emails with video links to educate him about what to expect in the hospital, milestone steps for discharge and the recovery journey.
Gold Stars:
- Orientation Timing: The virtual meeting was within a few weeks prior, so this gave us ample time to prepare in the days leading up to his surgery date.
- Orientation Content: The hip surgery nurse specialist reviewed pertinent information about what to expect before, during and after the surgery. The follow up emails including “Planning for your Recovery” provided essential information to get Sam’s home ready for his return post-surgery, addressing fall risks.
Magic Wand Wishes:
- Individual Patient & Caregiver Consultation: Since we had some questions that were specific to Sam’s situation, I wish that we had the option to schedule a virtual visit with the nurse to address our concerns in the days leading up to surgery. This would have reduced our anxiety around what to expect Sam to be able to do at different points of recovery.
Surgery
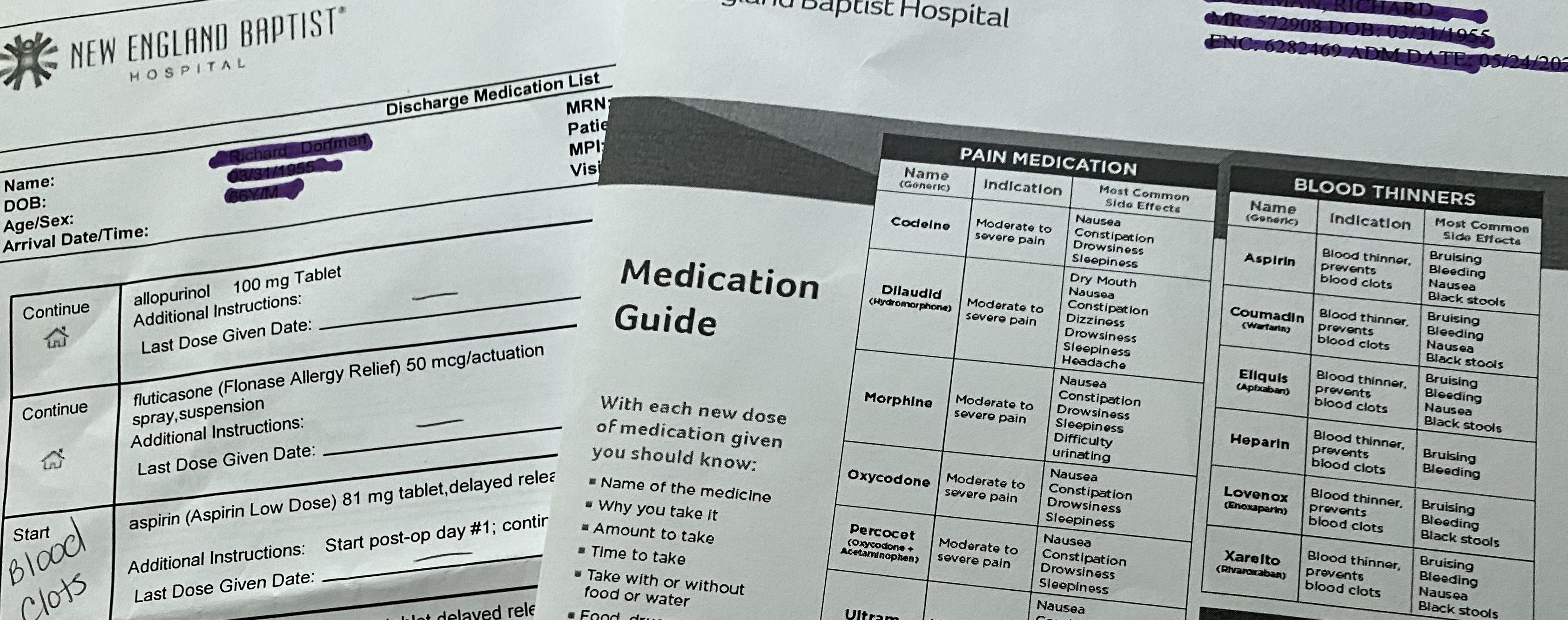 Discharge Medication informationDue to Covid, I dropped Sam off for pre-op with his crutches and cinch sack filled with paperwork and personal items for his stay. Several hours later, I was contacted by his nurse liaison about his status and about coming to his recovery room for a two- hour visit. It was not communicated to me or Sam if he would be staying over or being discharged. As 4pm neared, I asked about his discharge and the nurse moved quickly to get another PT session in to help Sam master stairs. The nurse went carefully through all discharge materials, answered all of our questions and then handed us the folder.
Discharge Medication informationDue to Covid, I dropped Sam off for pre-op with his crutches and cinch sack filled with paperwork and personal items for his stay. Several hours later, I was contacted by his nurse liaison about his status and about coming to his recovery room for a two- hour visit. It was not communicated to me or Sam if he would be staying over or being discharged. As 4pm neared, I asked about his discharge and the nurse moved quickly to get another PT session in to help Sam master stairs. The nurse went carefully through all discharge materials, answered all of our questions and then handed us the folder.
Gold Stars:
- Nurse Liaison: As Sam went through pre-op, he texted me a contact card for the nurse liaison, which gave me reassurance that I had someone to connect with about his surgery status.
- What to Expect Next Discussion: Instead of just telling us what we needed to do at home, the nurse walked us through the folder at discharge, reviewing each patient education insert so we understood what to do and where to go to re-read the information. This took the pressure off of us to remember everything that was mentioned during the discharge meeting.
Magic Wand Wishes
- What to Expect Packet/Medication: As a caregiver, I was disappointed that there were several different inserts related to medication (Med List, Medication Guide). Although it was quickly mentioned at discharge, it was not documented which medications are to be taken together (i.e. laxative with pain management meds). This would have helped us follow protocol. There also wasn’t a "medication tracking form", so as the caregiver, I had to create my own to record the times that each medication was given and indicate when medications were stopped. There is an opportunity for the provider to gather templates like this from other caregivers and provide them within the discharge packet.
Post-Surgery at Home
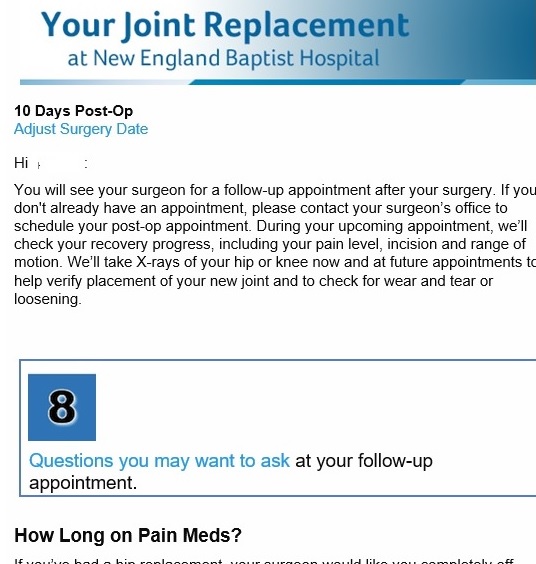 Post surgery emails tied to surgery date As promised at discharge, Sam received a call from VNA Care to schedule nurse and PT appointments. During these visits, Sam learned how he was doing, what was normal and required a call to the surgeon’s office. These visits have continued over the past few weeks, with the PT providing additional exercises for Sam to do in home.
Post surgery emails tied to surgery date As promised at discharge, Sam received a call from VNA Care to schedule nurse and PT appointments. During these visits, Sam learned how he was doing, what was normal and required a call to the surgeon’s office. These visits have continued over the past few weeks, with the PT providing additional exercises for Sam to do in home.
New England Baptist emails every few days to give us information about what to expect at that recovery point, which reduces our anxiety because we know what to look out for and how to respond.
Gold Stars:
- Care Coordination: Sam felt relieved that his care was continuous and the instructions consistent from the hospital to home, the discharge nurse to VNA Care nurse.
- Recovery perspective: Sam learned from his VNA Care nurse how he was healing relative to other patients. He felt relieved when he was able to master the PT exercises and he was off pain meds “much earlier than other patients” like him.
- Home Health Patient Education and Education Workbook: During the first VNA Care visit, the nurse handed us a 94-page book and pointed out pertinent pages for Sam and for me such as medication categorization and fall preventiion information. This helped us to not feel overwhelmed by the big workbook of information, especailly in the first few days when we are trying to address everything we need to do.
- Patient Education Journey: Sam and I find New England Baptist's post emails informative and relevent since they are tied to his surgery date and recovery milestones.
Magic Wand Wishes:
- Caregiver Post-Surgery Communication: With Sam on pain meds following surgery, it would have been helpful to have all patient communications also pushed to me/caregiver. After he was off of the pain meds and cognizant of what needed to be addressed, Sam forwarded the emails to me. I realized that several would have really been helpful such as what to look for and what to do in the first few days following surgery.
- VNA Visit Alerts: Although the nurse and PT mentioned that they were coming next Monday in the afternoon, it would have been helpful and expected for the patient and caregiver to receive a text reminder with the time range for their visit. Given that Sam is on crutches and often sitting with ice packs on his hip, I need to be available to answer the door for these visits.
- VNA Virtual Visit: As a caregiver, I had questions that needed to be addressed in between the VNA nurse visits. Although I was encouraged to call VNA Care at any time of day or night, I wished that I had the option of a virtual visit to show the nurse Sam’s swelling and bruising. This would have made me feel relieved since the nurse could have seen his hip and leg to make the best care decision instead of relying on my words to convey what I saw.
Caregiver Experience Opportunity
Although many health systems are focusing on the “patient experience”, few are addressing the "caregiver experience". Instead, they bring in the caregiver during Family Advisory Council sessions to gather input on specific initiatives.
Caregivers need the necessary communication, information and tools to be successful in supporting the care of their loved ones.
The caregiver must be included in the patient communications (with the patient’s permission) from surgery planning through recovery to ensure that the patient is prepared and following care related directions, especially regarding medications and exercises. Caregivers need to have access to professional caregivers to address questions and concerns. And they need to understand the relationship (roles and responsibilities) of the care entities as context for their communications. Does the VNA share Sam’s recovery information with his surgeon? Why is Sam’s health plan nurse calling? Does she have access to Sam’s VNA info? What can she address that the VNA nurse or the surgeon’s office cannot?
From an information standpoint, caregivers need clinical guidance (i.e. what is normal with swelling and bruising) as well as insights from other family caregivers. While supporting Sam through his recovery, I devised a long list of short cuts to make each day easier; from leaving pillow cases by the freezer for ice packs to placing water bottles at all of Sam’s sitting and sleeping spots for hydration to tricks for putting his compression socks.
In addition to tips from others, Caregivers can benefit from tools to support the patient care journey such as templates (e.g. medication tracking, recovery milestone checklist, calendar of what to do/stop doing in days leading up surgery). It is often one family caregiver who needs to keep other family members updated and these tools would help us feel more in control as we manage the journey from preparation through recovery.
Another beneficial tool would be a digital health app for the caregiver to track pain levels, swelling and other side effects, in between nurse visits to support interventions as needed. It is scary to be the one person who is responsible for noticing and responding to everything, especailly understanding how the symptoms are interrelated. Although the VNA Care nurse can address this when he is there, Sam's visits are only two times a week. What about all of the other days (and nights)? Yes we can call 24x7 but what if we miss sharing all pertinent information with the nurse?
Health systems can benefit from gathering information and tools from caregivers who have gone through the specific journey (hip replacement) and understand when these should be utilized and how they need to tie into the care flow with VNA Care and surgeon’s office.
Bringing caregivers into the communication loop and providing information and tools will empower them, save time and energy and generate both better outcomes and higher satisfaction ratings.
 Permalink
Permalink  June 9, 2021
June 9, 2021  Beginning Surgery ExperienceTwo weeks ago, Sam had hip replacement surgery at New England Baptist Hospital, a top nationally recognized orthopedic facility in Boston.
Beginning Surgery ExperienceTwo weeks ago, Sam had hip replacement surgery at New England Baptist Hospital, a top nationally recognized orthopedic facility in Boston. 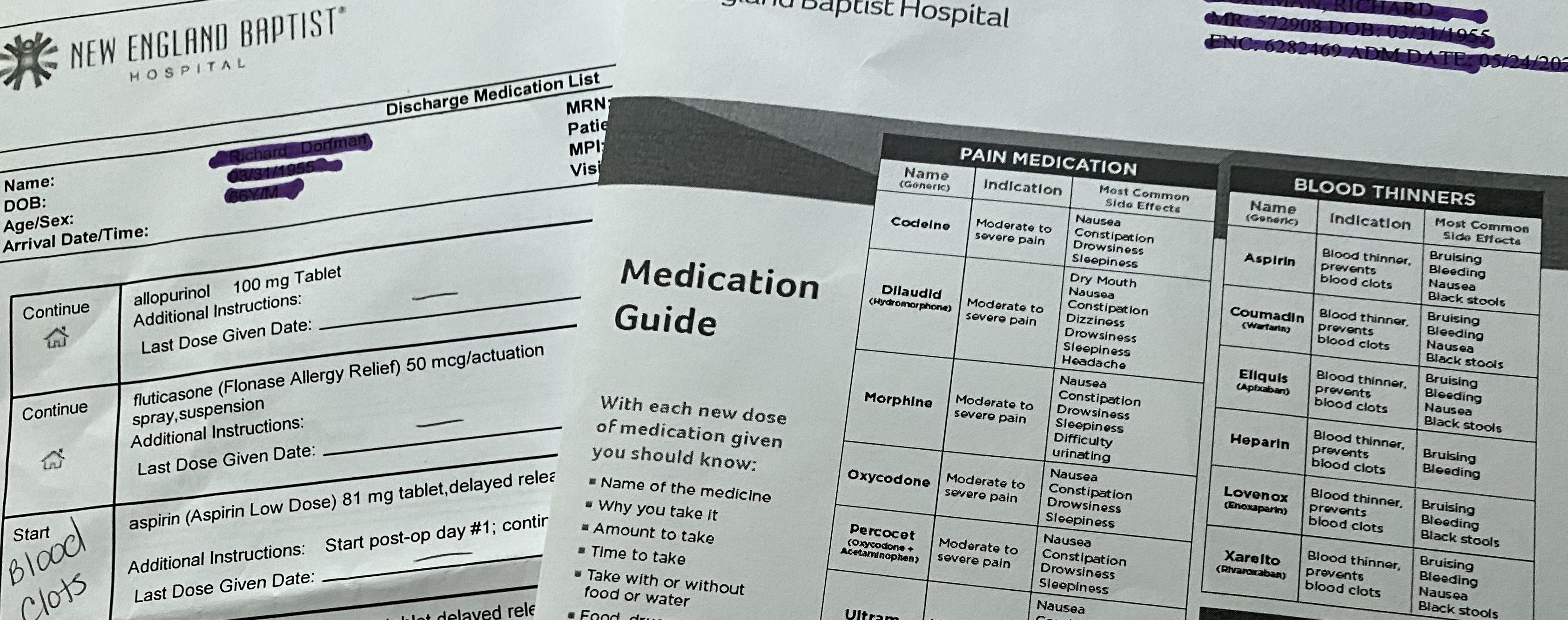 Discharge Medication informationDue to Covid, I dropped Sam off for pre-op with his crutches and cinch sack filled with paperwork and personal items for his stay. Several hours later, I was contacted by his nurse liaison about his status and about coming to his recovery room for a two- hour visit. It was not communicated to me or Sam if he would be staying over or being discharged. As 4pm neared, I asked about his discharge and the nurse moved quickly to get another PT session in to help Sam master stairs. The nurse went carefully through all discharge materials, answered all of our questions and then handed us the folder.
Discharge Medication informationDue to Covid, I dropped Sam off for pre-op with his crutches and cinch sack filled with paperwork and personal items for his stay. Several hours later, I was contacted by his nurse liaison about his status and about coming to his recovery room for a two- hour visit. It was not communicated to me or Sam if he would be staying over or being discharged. As 4pm neared, I asked about his discharge and the nurse moved quickly to get another PT session in to help Sam master stairs. The nurse went carefully through all discharge materials, answered all of our questions and then handed us the folder. 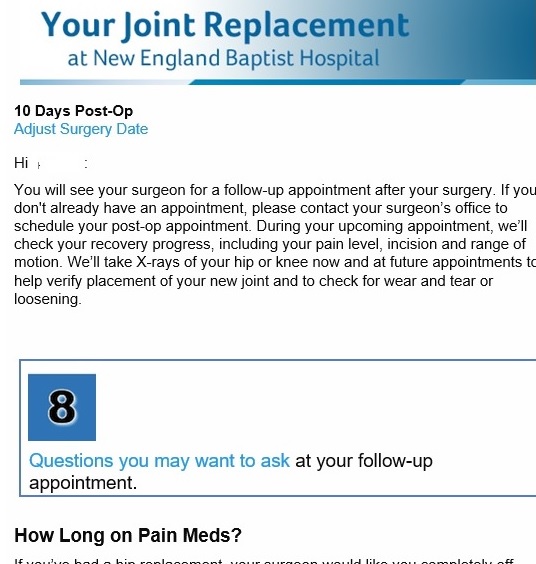 Post surgery emails tied to surgery date As promised at discharge, Sam received a call from VNA Care to schedule nurse and PT appointments. During these visits, Sam learned how he was doing, what was normal and required a call to the surgeon’s office. These visits have continued over the past few weeks, with the PT providing additional exercises for Sam to do in home.
Post surgery emails tied to surgery date As promised at discharge, Sam received a call from VNA Care to schedule nurse and PT appointments. During these visits, Sam learned how he was doing, what was normal and required a call to the surgeon’s office. These visits have continued over the past few weeks, with the PT providing additional exercises for Sam to do in home.