Twine Health Mobile App Engages Patients with Chronic ConditionsThe story about the health decline of our citizens is being told everywhere. According to the CDC website, “as of 2012, about half of all adults—117 million people—have one or more chronic health conditions. One of four adults has two or more chronic health conditions”.
Twine Health Mobile App Engages Patients with Chronic ConditionsThe story about the health decline of our citizens is being told everywhere. According to the CDC website, “as of 2012, about half of all adults—117 million people—have one or more chronic health conditions. One of four adults has two or more chronic health conditions”.
This negative trend is driving up healthcare costs and putting an ongoing strain on our healthcare system. A 2010 Robert Wood Johnson Foundation Report on Chronic Care: Making the Case for Ongoing Care states that eighty-five percent of all health care spending was on people with chronic conditions.
The positive part of the story is where the industry is heading. In the December 2014 PwC Health Research Institute (HRI) Report, two relevant health directions are described. The first is the “Do –It Yourself Healthcare movement” with implications for healthcare organizations to offer new patient engagement tools. The second is that “physician extenders see an expanded role in patient care”, where “doctor delegates” play an increasing role on the care team, which helps address physician shortages.
The real opportunity is at the intersection of the two, where patients use Do- It Yourself (i.e. self- management) tools which collect and communicate patient data (e.g. chronic condition vitals, medication adherence, lifestyle choices) to “doctor delegates”, who deliver guidance and support during the 99% of the time that the patient is living with his chronic condition.
Innovative healthcare organizations are experimenting with new technology tools and care delivery models to bring better care to their patient populations.
Care Collaboration for Hypertensive Patients
 Through Twine, patient collaborates with her nurse coach“We were looking for a way to help our Hypertensive patients get their blood pressure under control more quickly”, explains Dr. Katherine Rose, Brigham and Women’s Advanced Primary Care Associates, South Huntington. “When a patient is having trouble managing his blood pressure, we ask him to schedule a follow -up visit. We have found that some patients choose not to come in for another visit. When our nurses call patients to check- in on their blood pressure numbers, many patients don’t have them which limits the support that our nurses can provide”.
Through Twine, patient collaborates with her nurse coach“We were looking for a way to help our Hypertensive patients get their blood pressure under control more quickly”, explains Dr. Katherine Rose, Brigham and Women’s Advanced Primary Care Associates, South Huntington. “When a patient is having trouble managing his blood pressure, we ask him to schedule a follow -up visit. We have found that some patients choose not to come in for another visit. When our nurses call patients to check- in on their blood pressure numbers, many patients don’t have them which limits the support that our nurses can provide”.
The CDC confirms that hypertension is a growing problem in the U.S; “67 million adults (31%) have high blood pressure” and only about “half (47%) have their condition under control”.
Dr. Rose and her colleagues were determined to find a better way to support hypertensive patients through continuous communication and collaboration with their care team. “After evaluating different ways to leverage technology with a strong patient experience, we decided to use the Twine Health platform. In October 2014, we started a 6- month pilot and plan to recruit one hundred patients to participate”.
Twine Health is a spin- off from MIT Media Lab’s New Media Medicine Group. John O. Moore, MD, CEO and his team have designed the Twine solution with the goal of empowering patients to be an “apprentice”, learning to be “active participants in their care, particularly care of chronic disease”.
The Twine Collaborative Care Platform allows people to co-create a personalized care plan that serve as common ground for continuous collaboration with their care team; their own clinicians, family and friends, and a health coach (sometimes staffed by the clinic and sometimes provided on-demand by Twine).
Twine Health was awarded an opportunity to pilot as a winner of the Brigham and Women’s Hospital 2014 Pilot Shark Tank competition. “We are very excited about the Twine pilot,” shares Lesley Solomon, MBA, Executive Director of the Brigham Innovation Hub. “The Brigham is dedicated to providing outstanding patient care and we believe that innovative health IT solutions like Twine will help us to improve patient experience and engagement and better enable our clinicians to address complex clinical challenges. We look forward to seeing the results of this pilot."
Hypertensive Patient Pilot
Dr. Rose explains that initially patients in her practice were recruited during an office visit. After hearing about Twine Health from her doctor, an interested patient worked closely with the Nurse to download the mobile app to her phone, set up her care plan, goals and select daily activities to support self- management.
Patient recruitment efforts are being accelerated through an email campaign with a link to the Twine mobile app and through television promotional messages in the waiting room. These communications show patients how to use the Twine Health mobile app to receive ongoing support and guidance from their nurse at the practice. Patients learn that they do not need to come in for all of their visits and can communicate their blood pressure readings and health behaviors digitally for continuous care.
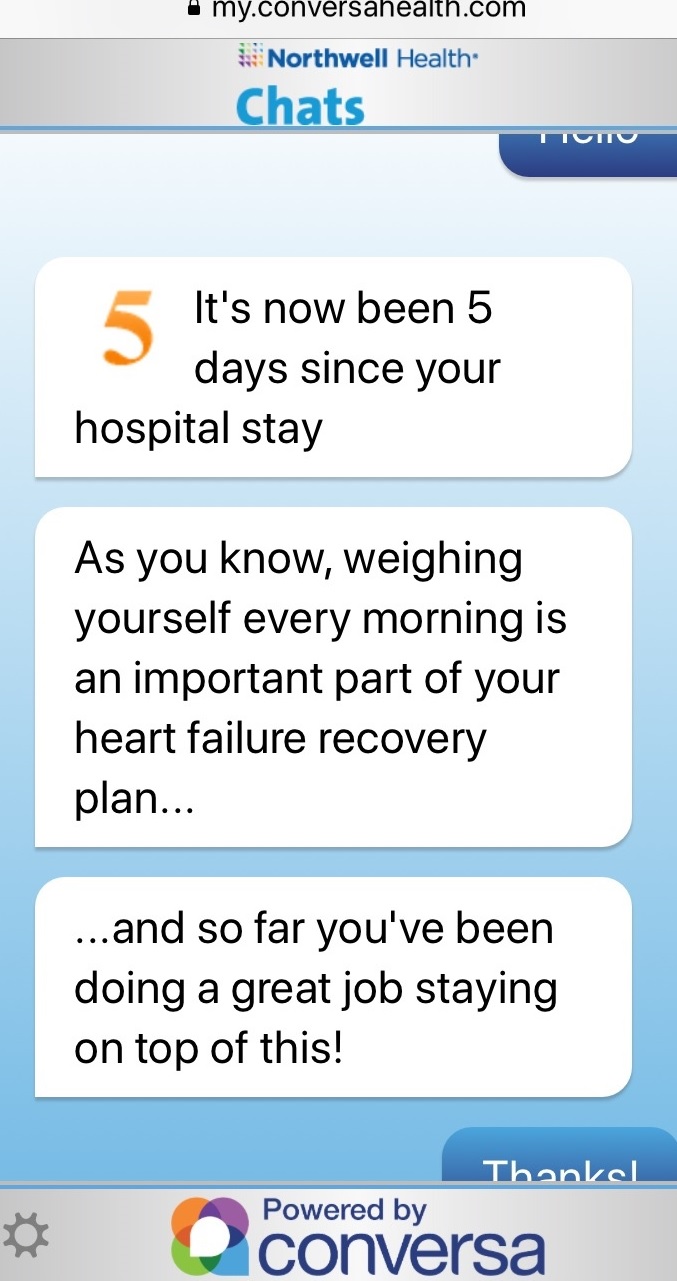
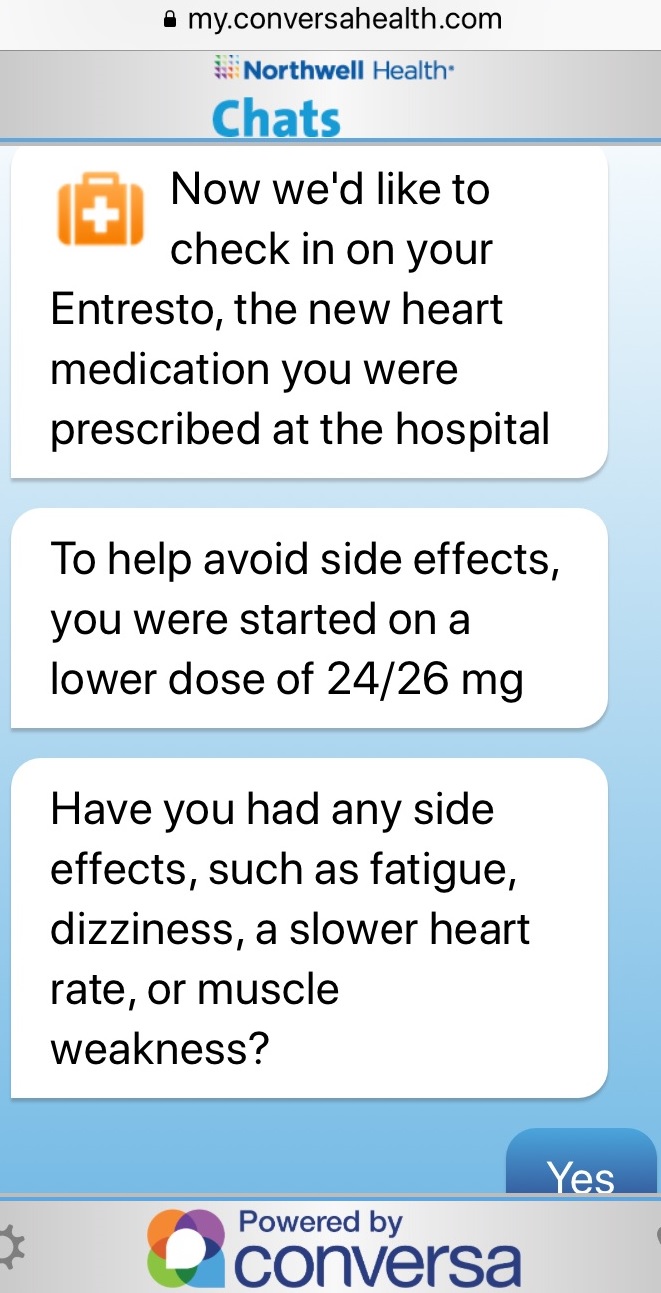
Once enrolled in the Twine Health program, patient Patricia can view her daily care plan and check off activities which include completing certain activities (e.g. taking medications, walking, relaxing) and avoiding others (e.g. not eating salty foods, reducing alcohol consumption). Patricia can elect to receive reminders to take her medications, log her blood pressure readings and walk at lunch. She can monitor progress towards her goal and send a secure message to her nurse.
 Nurse monitors chronic patients needing motivation and supportNurse Nancy monitors the Twine Health dashboard to see her patient’s care plan progress and identify patients that need support (e.g. missed medications, failed to measure blood pressure, blood pressure measure out of range). Nancy sees patient’s blood pressure readings, number of days adherent and days remaining on the patient’s care plan and quickly answers patient’s questions or concerns (e.g. running out of medication, experiencing medication side effects). She sends congratulatory messages to Patricia and other patients reaching goals and encouraging messages to less engaged patients to come back onto Twine to share information and issues. Nurse Nancy creates new and modifies existing care plans working closely with her patients. She also uses the platform to check in with the patient’s doctor about care plan and medication changes.
Nurse monitors chronic patients needing motivation and supportNurse Nancy monitors the Twine Health dashboard to see her patient’s care plan progress and identify patients that need support (e.g. missed medications, failed to measure blood pressure, blood pressure measure out of range). Nancy sees patient’s blood pressure readings, number of days adherent and days remaining on the patient’s care plan and quickly answers patient’s questions or concerns (e.g. running out of medication, experiencing medication side effects). She sends congratulatory messages to Patricia and other patients reaching goals and encouraging messages to less engaged patients to come back onto Twine to share information and issues. Nurse Nancy creates new and modifies existing care plans working closely with her patients. She also uses the platform to check in with the patient’s doctor about care plan and medication changes.
Pilot Considerations
Dr. Rose and her colleagues worked closely with the Twine team to plan their pilot.
Participant Selection:
“Not all of our patients have a smart phone which is required to access the Twine Health platform. We also needed to choose patients who would feel comfortable using a smart phone to support and extend their care. Since Twine is currently available in English, we are only offering it to selected patients”, Dr Rose explains.
Nurse Selection:
“As we thought about the role of coaching and motivating our patients to better manage their hypertension, we decided to use our LPNs to support the Twine Health program. Our LPNs interface with our patients all the time and are often on their computers doing triage. At our practice, we also like to have our professional team members operating at their top of license.”
EMR Inclusion:
Dr. Rose wanted to incorporate summarized patient data information into their EMR and appreciated that Twine Health created a note template to capture changes in the care plan, goals and medications. The nurse copies and pastes this information into the EMR so that everyone can access the latest patient care information.
Pilot Evaluation
At the end of the 6- month pilot, Dr. Rose and her team will review qualitative and quantitative feedback from patients and clinicians. “We will also look at measures to see how often the patient’s blood pressure was controlled, how many blood pressure check visits were avoided, how engaged the patients were (e.g. use the platform, make better lifestyle decisions) and how satisfied patients felt (i.e. their team took better care of them).
Patient Feedback
Patients appreciate encouraging feedback from their nurse, find it motivating and feel a sense of achievement when reaching their goal. They also like being able to ask the nurse questions through the app that they may not have otherwise asked.
“Our patients are helping us enhance Twine. For example, a patient suggested that we expand the capability to add blood pressure measurements more than once a day” describes Dr. Rose.
Clinician Feedback
The clinicians using Twine value understanding what is happening to the patient outside of the office visit to provide ongoing support. From a clinical perspective, Dr. Rose shares “I am excited that the app gives the patient ownership of their health. While working with one patient on his care plan, he suggested increasing the time on his stationary bike to avoid adding a medication. Since extending his exercising will help more than just his blood pressure, I was all for it”.
The Twine platform gives clinicians at the Brigham and Women's practice valuable visibility into the barriers that impact the patient’s adherence. With this insight, nurses are able to better understand and provide more relevant guidance to support the patient holistically for better outcomes.
Dr. Rose explains “there are many reasons why patients are unable to take their medications. Some are simple—the pharmacy didn’t get the prescription, and others are more complex—the patient has concerns about a possible side effect. As providers, we sometimes don’t hear about the problem for a couple of months which is lost time. With improved communication tools, we can address problems immediately, hopefully improving compliance and health outcomes”.
With only two months into the Twine Health Pilot, Dr. Rose admits that they are just beginning.
“We will be looking at the financial impact of using the Twine platform. So far we know that our nurses are spending 20- 30 minutes to set up each patient and 25- 30 minutes daily responding to and motivating patients,” confides Dr. Rose.
She appreciates that Twine Health conducts conference calls with other healthcare organizations participating in pilot programs to learn ‘best practices’ together such as incorporating Twine into existing workflows, recruiting patients, engaging patients and trying an approach for a specific patient segment.
“Ultimately we think that patients who are more engaged in their care and mindful of their choices will be healthier. We are excited to use new technologies like Twine to encourage that”, Dr. Rose concludes.
Interested in seeing Twine Health results across all hypertensive patients? Twine displays this on an aggregate level through their online dashboard.
 Motivation for health and wellness,
Motivation for health and wellness,  educating consumers about health and wellness,
educating consumers about health and wellness,  online health and wellness coaching,
online health and wellness coaching,  patient education,
patient education,  patient experience,
patient experience,  patient journey,
patient journey,  personalization for health and wellness in
personalization for health and wellness in  AI consumer engagement,
AI consumer engagement,  Care collaboration,
Care collaboration,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Personalization eHealth,
Personalization eHealth,  patient health education
patient health education